In recent years, U.S. maternal mortality has become a pressing public health concern, as the country continues to experience alarmingly high rates of pregnancy-related deaths among high-income nations. Despite over 80 percent of these fatalities being preventable, significant disparities persist across various demographics, particularly race and geography. A study conducted between 2018 and 2022 revealed that factors including inadequate prenatal care and insufficient postpartum support contribute to this ongoing crisis. Particularly concerning is the impact of the COVID-19 pandemic, which exacerbated existing maternal health disparities and led to a sharp increase in mortality rates. Addressing these issues is essential to safeguard maternal health and ensure that all women receive equitable care throughout their pregnancy and postpartum journey.
Maternal health outcomes in the United States, particularly concerning maternal death rates, highlight a critical area of public health that requires attention. The increasing incidence of maternal fatalities during and after pregnancy raises alarms about the effectiveness of current healthcare systems and policies. Vulnerable populations, especially women of color and those in healthcare-deprived regions, face substantial challenges during their prenatal and postnatal periods. Furthermore, the lingering effects of the COVID-19 pandemic have significantly complicated the landscape of maternal healthcare, revealing the necessity for a comprehensive approach to prevent pregnancy-related deaths. This discussion aims to delve into the factors influencing maternal health disparities and explore effective strategies for improving outcomes for all mothers.
Understanding U.S. Maternal Mortality Rates
The United States has long struggled with high maternal mortality rates compared to other high-income countries. Recent studies have revealed alarming trends, with pregnancy-related deaths showing an upward trajectory from 2018 to 2022. A shocking fact is that over 80% of these deaths are preventable, highlighting the urgent need for systemic improvements in maternal healthcare. The data indicates that during this period, American Indian and Alaska Native women faced the highest mortality rates, exposing significant healthcare disparities based on race and ethnicity.
Complex factors contribute to these high rates, including systemic inequities within the healthcare system, socioeconomic factors, and the prevalence of chronic illness among women of reproductive age. For instance, cardiovascular diseases have emerged as the leading cause of maternal mortality, eclipsing other causes like hemorrhage. This shift underscores the importance of addressing chronic health conditions that can arise before, during, and after pregnancy, necessitating targeted interventions.
Frequently Asked Questions
What are the primary causes of U.S. maternal mortality during pregnancy?
In the U.S., the leading causes of pregnancy-related deaths include cardiovascular disease, hemorrhage, and hypertensive disorders such as pre-eclampsia and eclampsia. Alarmingly, cardiovascular disease now accounts for over 20% of these deaths, highlighting the need for improved maternal health care and risk management throughout pregnancy and the postpartum period.
How does the U.S. maternal mortality rate compare to other high-income countries?
The U.S. has the highest maternal mortality rate among high-income countries, with studies showing a continuous rise from 2018 to 2022. This is attributed to factors such as an inequitable healthcare system, lack of adequate prenatal and postpartum care, and persistent health disparities based on race and ethnicity.
What impact did COVID-19 have on maternal health and pregnancy-related deaths in the U.S.?
The onset of the COVID-19 pandemic in 2020 was linked to a sharp increase in pregnancy-related deaths, particularly in 2021. Subsequently, while there was a slight decline in rates, maternal mortality in 2022 remained higher than in 2018, indicating the pandemic’s lasting impact on maternal health.
What role do maternal health disparities play in the rising U.S. maternal mortality rates?
Significant disparities exist in U.S. maternal mortality rates based on race and ethnicity. For example, American Indian and Alaska Native women face mortality rates nearly four times higher than white women. These disparities underscore the urgent need for targeted interventions in maternal healthcare to ensure equitable access and outcomes for all women.
How important is postpartum care in reducing U.S. maternal mortality?
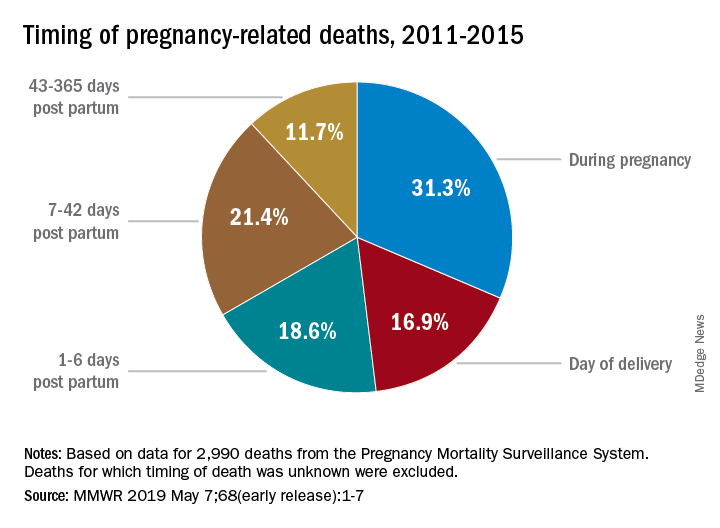
Postpartum care is critical, as nearly a third of maternal deaths occur between 42 days and one year postpartum. Extending care beyond six weeks and addressing health issues during this period can significantly improve maternal health outcomes and reduce mortality rates.
What preventative measures can reduce pregnancy-related deaths in the U.S.?
Preventative measures include enhancing access to quality prenatal and postpartum care, addressing chronic health conditions among pregnant individuals, and implementing equitable healthcare policies. Additionally, investing in public health infrastructure and reducing disparities in maternal healthcare can mitigate risks associated with pregnancy-related deaths.
What is the significance of late maternal deaths in the context of U.S. maternal mortality?
Late maternal deaths, occurring between 42 days and one year after pregnancy, are significant as they signal the need for comprehensive healthcare strategies that extend beyond the postpartum period. Acknowledging this timeframe can help in designing better support systems for women after childbirth.
How can U.S. maternal mortality rates be improved through policy changes?
Improving U.S. maternal mortality rates requires comprehensive policy changes that include increasing funding for maternal health programs, standardizing healthcare practices across states, and focusing on reducing racial and state-level disparities in care and medical outcomes.
What is the current trend in U.S. maternal mortality rates over recent years?
Recent trends indicate a troubling rise in U.S. maternal mortality rates, with figures showing an increase from 25.3 to 32.6 deaths per 100,000 live births between 2018 and 2022. This upward trend highlights the urgent need for action to enhance maternal health services.
What innovations are being proposed to address U.S. maternal health issues?
Proposed innovations include integrating comprehensive maternal health services that address physical, emotional, and social aspects of care, investing in telehealth options, and creating community-based interventions to support expectant and postpartum mothers, ultimately aimed at reducing pregnancy-related deaths.
| Key Point | Details |
|---|---|
| Rising Maternal Mortality | The U.S. has the highest maternal mortality rate among high-income countries, which increased from 25.3 to 32.6 deaths per 100,000 live births from 2018 to 2022. |
| Preventable Deaths | More than 80% of pregnancy-related deaths in the U.S. are preventable. |
| Racial Disparities | Significant disparities exist, with rates for American Indian and Alaska Native women at 106.3 deaths per 100,000 live births compared to 27.6 for white women. |
| Healthcare System Issues | Factors include a patchwork healthcare system, inequitable policies, and existing biases. |
| Chronic Conditions | Increasing rates of chronic conditions, such as hypertension, in younger people are contributing to rising mortality rates. |
| Late Maternal Deaths | Late maternal deaths (42 days to 1 year post-pregnancy) account for nearly a third of pregnancy-related deaths. |
| Need for Public Health Investment | Continued investment is critical for improving maternal health outcomes and addressing disparities. |
Summary
U.S. maternal mortality is a critical public health issue, highlighted by preventable deaths and stark racial disparities in outcomes. Despite some innovations, the U.S. continues to lag behind other high-income nations in maternity care, necessitating urgent investments in both prenatal and postpartum healthcare to reverse the troubling trajectory of rising mortality rates.